Maintain Member Eligibility
With new redetermination and work requirements, maintaining member eligibility for Medicaid insurance coverage will become a primary social need. As the leaders in solving social needs, we identify barriers and remove obstacles that prevent people from accessing the care they deserve.

Personalized engagement for all members, direct support for high-risk population
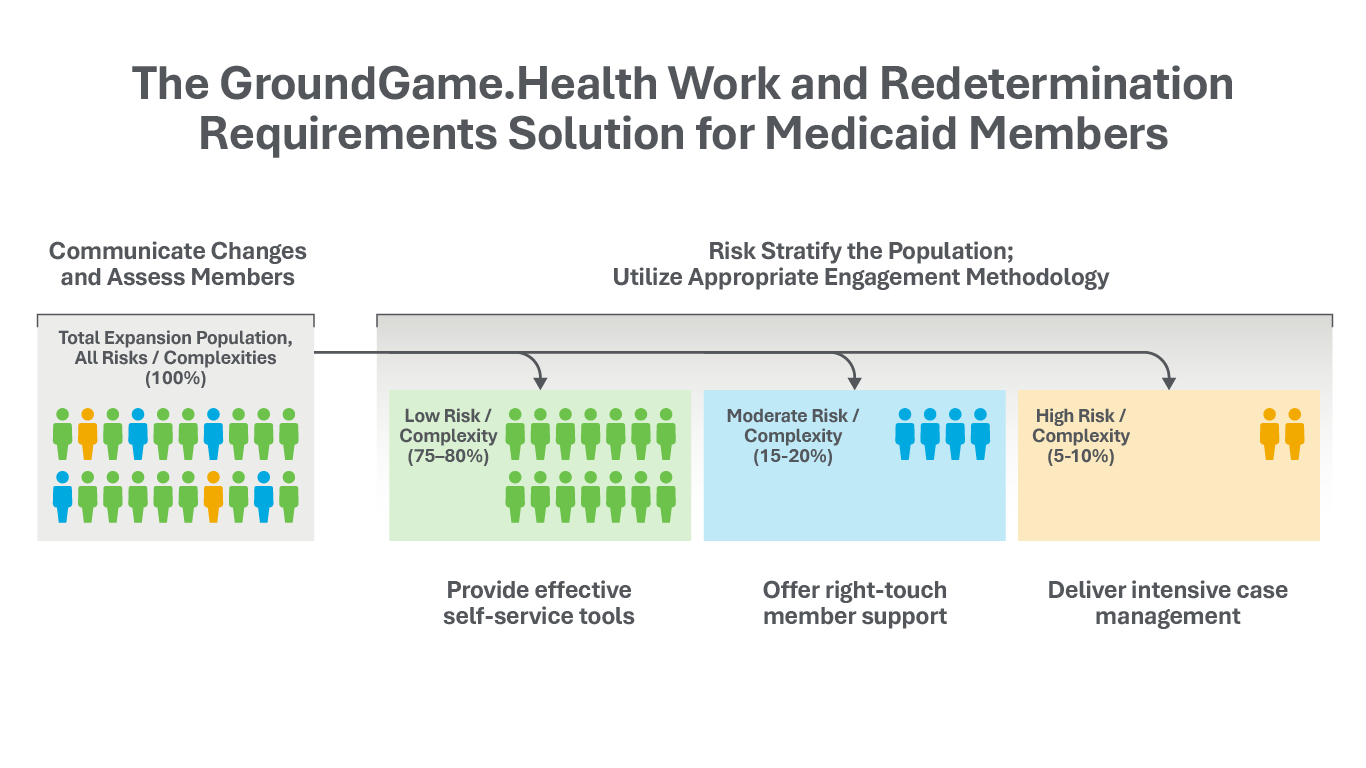
We create an N of 1, culturally tailored, personalized member experience, powered by our Right Touch engagement model that drives results through our deep relationships within a curated network of community-based organizations (CBOs) across the country.
With our solution for addressing new work and redetermination requirements for Medicaid members, we leverage our deep experience reaching and engaging with health plan members to drive action.
By strategically stratifying members according to risk and complexity, we ensure that the right information reaches the right members, at the right time.
Thought leadership
GroundGame.Health experts weigh-in on the new redetermination and work requirements for Medicaid members, and provide deep insights on the impacts, and how to navigate these changes.

White Paper: How Medicaid payers can prepare
Big changes are coming, and payers need to act now. Learn from the experts how to navigate the upcoming Medicaid work requirements landscape.

Under the Same Sky: Jackie Prokop
Abner Mason spoke with Jackie Prokop, Associate Principal, HMA, who discussed the complexities of designing and deploying work requirements programs based on her firsthand insights from Michigan's 2020 rollout.
Under the Same Sky: Jacey Cooper
Abner Mason spoke with Jacey Cooper, President, Precision Health Strategies, who drew examples from her extensive background in transformational initiatives, outlining three critical strategies for states and health plans navigating this evolving landscape.
Under the Same Sky: Karen Shields
Abner Mason spoke with Karen Shields, CEO of KMS Health Consulting, who provided key lessons learned from her experience with the rollout of the Affordable Care Act (ACA) as well as Medicaid unwinding.
Under the Same Sky: John Morales
Abner Mason spoke with John Frias Morales, an analytics expert, who discussed how states and health plans can avoid built-in bias and design systems that help Medicaid beneficiaries retain their health insurance coverage.
Under the Same Sky: Jessica Kahn
Abner Mason spoke with Jessica (Jess) Kahn, Partner at McKinsey based out of Washington, D.C. Jess shared practical advice drawn from her decades of experience in state and federal government and in her current role as a partner at McKinsey.
Article Series
GroundGame.Health's own Syam Adusumilli, Chief Evangelist and Head of Strategic Partnerships, has initiated a series of articles with useful perspectives and insights on these new requirements.
To help you navigate relevant articles, reference the following pathways guide.
• Health Plan Executives: Recommend article series 3, 12, and 11
• State Regulators: Recommend article series 7, 13, and 14
• Community Organization Leaders: Recommend article series 8, 11, 15E, and 15F
• Provider/Health Systems: Recommend article series 9 and 11
• Employers: Recommend article series 5 and 12
• Educational Institutions: Recommend article series 10
• Policy Researchers: Recommend article series 15 and 16
• Navigator/Frontline Workers: Recommend article series 2C, 8, and 11
1A: The New Social Contract: From Safety Net to Trampoline
The One Big Beautiful Bill Act represents more than budget policy, it's a fundamental reordering of the relationship between citizens and their government.
1B: The New Stakeholders: Who Implements the Distributed Social Contract
When work becomes a condition of healthcare coverage, responsibility spreads far beyond government agencies.
1C: The Systems View: How Work Requirements Create Unpredictable Outcomes
When Arkansas implemented Medicaid work requirements in June 2018, state officials anticipated promoting employment and personal responsibility. What they got instead was 18,000 people losing coverage in ten months — with no measurable increase in employment.
2A: Building Verification Systems that Work: Technology’s Role in the Reciprocal State
When 18.5 million people must document 80 hours of activity monthly, system design becomes social policy.
2B: Exemption Systems and the Boundaries of Obligation
Who shouldn't have to work, who decides, and how do we know?
2C: The Human Layer: Agency, Advocacy, and Community Engagement
Systems don't implement themselves — people make them work, or make them fail.
3A: What Health Insurers Can Do: Turning Enrollment Volatility Into Care Continuity
The question isn't whether work requirements are good policy. The question is what operationally competent managed care organizations do when policy creates volatility that threatens both business models and population health.
3B: The 14-month Implementation Checklist: What MCOs Must Do Now
The plans that execute well aren't those with the most resources. They're those that started earliest and iterated fastest. Start now.
3C: Managing the Multiple Burdened: Care Coordination when Medical Risk, Social Complexity,and Administrative Barriers Converge
Effective MCO response doesn't create ten different programs. It creates flexible, adaptive support systems that accommodate intersectional complexity
4A: The Expansion Redetermination Challenge for Adults
Redetermination for adults goes beyond monthly work verification, serving as a periodic, comprehensive review of Medicaid eligibility, including income, household changes, and continued compliance with work or exemption requirements.
4B: When Redetermination Meets Reality
What happens when Medicaid redetermination deadlines collide with mental illness, disability, and caregiving? For thousands of expansion adults, a six-month cycle meant to verify eligibility becomes a recurring crisis costing coverage, health, and sometimes lives.
4C: Building Redetermination Infrastructure for Expansion Adults
States face a 14-month deadline to overhaul Medicaid systems for 18.5 million expansion adults. Semi-annual redetermination isn’t just a policy shift, it’s a capacity crisis requiring new technology, staffing, and coordination across every stakeholder.
4D: When the Disability Itself Prevents Documentation: Autism, IDD, and the Redetermination Penalty
For adults with autism and intellectual disabilities and their caregivers, the six-month Medicaid redetermination cycle isn’t just paperwork, it’s a barrier that punishes the very conditions exemptions are meant to protect.
5A: Employers as Safety Net Partners: The Private Sector's New Role
When a paystub becomes a passport to healthcare, employers inherit responsibilities they never requested and opportunities they may not yet recognize.
5B: The Employer Segmentation Challenge
Large corporations, mid-sized firms, self-insured employers, small businesses, Taft-Hartley plans, and public sector organizations face fundamentally different opportunities and constraints in supporting expansion adult employees.
5C: The Unstable Employment Reality
The gap between being employed and meeting 80 monthly hours reflects structural features of low-wage labor markets, not individual work ethic failures .
5D: Employer Liability and Reluctance
Employers are being conscripted as verification infrastructure without their consent, creating resistance that ranges from passive non-cooperation to active avoidance.
5E: Union and Collective Bargaining Dimensions
Unionized workers face distinct work requirement dynamics shaped by collective bargaining agreements, seniority systems, and union hall infrastructure.
6A: The Expansion Dual Challenge
For a few hundred thousand Americans who entered Medicaid through expansion before qualifying for Medicare disability, work requirements create unprecedented complexity
6B: Managing Dual Eligibles Under Work Requirements: What D-SNPs and States Must Do
Operational strategies for serving the most complex population facing the most complex policy.
7A: The Exemption Architecture
Exemption rules are more than paperwork. They reflect choices about trust, capacity, and the purpose of safety nets, shaping whether Medicaid work requirements expand opportunity or restrict coverage.
7B: The Verification Architecture
The Verification Architecture is the arena where states confront the choice between trusting systems or trusting people, a decision that defines not only administrative design but the very balance between oversight, burden, and coverage stability.
7C: The Coordination Architecture
The sequencing of bureaucratic processes determines whether compliance unfolds as a stable transition or fractures into systemic failure.
7D: The Delegation Architecture
Building Medicaid delegation systems means more than logistics. It requires attention to safe harbors, constitutional limits, and liability protections that determine whether employers, providers, and schools can truly participate.
8A: Faith-Based Organizations as Trusted Intermediaries
How spiritual authority, regular connection, and congregational life create unique capacity for work requirement navigation.
8B: Grant-Funded CBOs and the Mission Drift Problem
When community organizations assume government contracts, they face tensions in balancing service provision with advocacy and in sustaining funding while preserving organizational autonomy.
8C: Community Inclusive Social Enterprises as Reciprocal Infrastructure
When peer support becomes paid work, community capacity is built through mutual aid.
8D: Decentralized Autonomous Organizations and Programmable Support
When coordination happens through code: using blockchain, smart contracts, and AI agents to enable peer navigation without centralized institutional control.
8E: The Competency Matrix: Matching Capabilities to Complexity
How navigation support works through competency-based matching rather than organizational tiers.
8F: The Ecosystem in Practice: Limitations
What navigation actually looks like from the recipient's perspective, how coordination happens across organizational boundaries, who builds the technology layer, and what accountability means when no single entity controls the system.
8G: The Rural CBO Capacity Crisis
Rural areas facing work requirements often lack the community organization infrastructure that urban implementation models assume.
8H: Informal Mutual Aid Networks
As expansion adults already rely on informal mutual aid networks for survival, formalizing these networks enough to count for verification without destroying their informal character could leverage existing community capacity.
9A: Accountable Care Organizations and Work Requirements
How work requirements destabilize ACO's and what payment, governance, and data reforms are needed to protect care for vulnerable populations.
9B: Physician Practices and the Exemption Burden
When clinical care meets administrative gatekeeping.
9C: Hospital Systems as Work Requirement Infrastructure
When institutional missions collide with eligibility instability.
9D: Provider Attestation Liability
What healthcare providers risk when they document work exemptions.
9E: Provider Tax Restrictions and State Implementation Capacity
How the Medicaid financing freeze constrains work requirement infrastructure.
9F: Pharmacies as Work Requirement Touchpoints
Pharmacies see Medicaid patients more frequently than any other healthcare touchpoint, creating opportunities for coverage loss early warning, exemption identification, and navigation access.
9G: Behavioral Health Provider Perspectives
Behavioral health providers face unique tensions in work requirement implementation: confidentiality requirements, episodic conditions, and therapeutic relationships that administrative gatekeeping can undermine.
10A: Higher Education as Compliance Infrastructure
How community colleges, public universities, and online programs become essential work requirement pathways.
10B: Vocational Training and Workforce Development
How vocational training, apprenticeships, and workforce development programs can serve as practical pathways for Medicaid work requirement compliance.
10C: GED, ESL, and Adult Basic Education
Why GED, ESL, and adult basic education, as well as the infrastructure to verify them, are critical to real compliance and economic mobility.
10D: Navigator Training, Volunteer Training, and Job Readiness Programs
How navigator, volunteer, and job readiness programs build human capital while strengthening work requirement systems.
10E: The Technical Framework
Turning credit hours into compliance: the technical rules that make education a real pathway.
10F: Supporting the Education Ecosystem
Coordinating investments across MCOs, hospitals, employers, and community partners to turn education into a sustainable compliance pathway.
10G: When Education Counts But Financing Evaporates
Federal policy encourages education for coverage while simultaneously dismantling the borrowing system that funds graduate programs, leaving students with rules that promise opportunity but deliver barriers.
10H: The For-Profit Education Problem
When education becomes a compliance product, vulnerable adults face aggressive marketing, high costs, and credentials that lead nowhere.
10I: Education Employment Transitions
Work requirements reward training but ignore transition realities, creating coverage loss at the moment of success.
11A: Pregnant and Postpartum Populations
Rigid exemption systems collide with biological complexity, turning maternity care into an administrative gauntlet instead of a protected pathway.
11B: Serious Mental Illness and Work Requirements
Policies built on the expectation of stability fail when serious mental illness creates fluctuating realities, leading to coverage gaps during critical episodes.
11C: Substance Use Disorders and Recovery Pathways
Strict compliance rules clash with the chronic and unpredictable nature of addiction, turning routine administrative deadlines into pressure points that can trigger relapse and destabilize recovery.
11D: Justice-Involved and Reentry Populations
Verification systems built for predictability clash with the realities of reentry, where criminal records, probation demands, and untreated health conditions make meeting 80-hour work requirements nearly impossible.
11E: Homelessness and Work Requirements
When verification systems demand addresses, phones, and paystubs, homeless populations face coverage loss that drives higher emergency costs and worse health outcomes.
11F: Caregiving Responsibilities and Work Requirements
Exploring how rigid verification systems ignore caregiving realities, forcing coverage loss for millions providing essential family care.
11G: Transition Scenarios and Cliff Effects
Why predictable life events like birthdays, treatment completion, and caregiving changes create preventable coverage loss and how grace periods, graduated requirements, and proactive planning can stop it.
11H: Populations Requiring Confidentiality Protections
Work verification systems that prioritize disclosure over safety put survivors and other vulnerable populations at risk. States must implement confidentiality protections through sealed records, alternative verification methods, and trauma informed processes to ensure security and coverage continuity.
11I: Geographic and Digital Isolation
When rural isolation and lack of digital access make compliance impossible, states must adopt flexible hour requirements, seasonal averaging, and multiple verification channels to prevent coverage loss.
11J: Limited English Proficiency and Cultural Barriers
Language barriers and informal employment patterns make standard work verification ineffective, requiring states to provide professional translation, bilingual navigation, and alternative documentation methods to maintain coverage.
11K: Non-SSI/SSDI Qualifying Disabilities
Partial disabilities leave millions able to work but unable to meet uniform 80-hour requirements, making graduated thresholds and functional capacity assessments critical to preserving coverage.
11L: Intersectionality and Multiple Simultaneous Barriers
Compounding barriers across health, caregiving, geography, and language turn compliance into impossibility, requiring total burden assessments and graduated requirements to preserve coverage.
11M: Veterans with Service Connected Disabilities
Veterans with service-connected disabilities often fall short of uniform 80-hour work requirements despite documented limitations, making integration of disability ratings, recognition of treatment time, and transition grace periods essential to prevent coverage loss.
11N: LGBTQ+ Populations and Work Requirements
When discrimination limits employment options, meeting hour thresholds becomes harder than policy imagines.
11O: Populations with Complex Medical Conditions
For people with complex medical needs, the time spent on appointments, treatments, and medication management often exceeds what systems recognize as productive activity.
11P: Foster Care Alumni and Work Requirements
Work requirements collide with the realities of foster care alumni, where trauma, housing instability, and lack of family support turn small setbacks into catastrophic spirals.
11Q: Agricultural and Seasonal Workers
Seasonal farm work follows crop cycles rather than monthly calendars, leaving workers who far exceed annual hour thresholds vulnerable to losing coverage during predictable gaps.
11R: The Structurally Locked Out
A significant population of expansion adults who work consistently are unable to reach 80 monthly hours due to employer decisions, labor market structure, or economic constraints rather than personal limitations.
11S: Appalachian and Post-Industrial Communities
In regions where deindustrialization has collapsed labor markets, work requirements become not behavioral intervention but administrative mechanism for coverage loss.
12A: The Economics of Mutual Obligation: Who Pays, Who Saves, Who Bears the Risk
Projected savings from Medicaid work requirements often overlook the cascading costs they create such as administrative complexity, enrollment churn, uncompensated care, and disrupted payment models, raising the fundamental question of who pays, who saves, and who bears the consequences.
12B: Weighted Hours and Activity Credits: Design Frameworks for Differentiated Requirements
When states design work requirement systems, choices about equal hours, weighted activities, and barrier adjustments determine whether policies promote workforce attachment, human capital investment, or coverage stability, shaping outcomes as much as the mandate itself.
12C: Navigation Infrastructure ROI Analysis: Comparing Investment Models for Work Requirement Support
Deciding between professional navigators, community enterprises, and volunteer networks will determine whether work requirements protect coverage or create gaps.
12D: December 31st Financial Cliff Analysis: When Medicaid Ends and Nothing Replaces It
How Medicaid work requirements create a coverage void, leaving millions uninsured as the safety net disappears.
12E: The Retention Paradox: Risk Adjustment, Redetermination and Work Requirements
Why your most difficult members are your most valuable.
12F: The December 2025 Convergence: When Multiple Policy Cliffs Collide
How overlapping policy cliffs such as expiring ACA subsidies, new Medicaid work requirements, housing voucher cuts, and student loan pressures create a perfect storm of financial instability for millions
13A: The Documentation Gap
When Medicaid work requirements punish paperwork failures instead of work failures.
13B: When December 2026 Won't Work: Extension Requests and Interim Status
Inside the scramble for extensions as states confront impossible timelines and inadequate systems.
13C: Behavioral Economics of Compliance
Compliance isn’t a test of character, it’s a design challenge. Behavioral science shows how to build systems that help people succeed
13D: Gaming, Fraud, and Program Integrity
Program integrity that protects coverage: targeting real fraud without punishing the compliant.
13E: Four Work Requirements, One Person
Compliance across SNAP, Medicaid, childcare, and housing: a burden that undermines the very stability these programs promise.
13F: Technology Vendor Landscape
When states must choose between building, buying, or blending technology for Medicaid work requirements under impossible timelines and fragmented vendor markets.
13G: The Marketplace Fallback Problem
The marketplace was meant to be a safety net for those leaving Medicaid but work requirement penalties and subsidy exclusions turn that bridge into a dead end for millions.
14A: Great Lakes
An in-depth look at how Great Lakes states (Illinois, Indiana, Michigan, Minnesota, Ohio, Wisconsin) are navigating federally mandated Medicaid work requirements amid political divides, economic shifts, and social equity challenges.
14B: Gulf South
Exploring how Arkansas, Louisiana, Mississippi, and Texas confront Medicaid work requirements, expansion gaps, and the deep structural forces shaping healthcare access across the Gulf South.
14C: Mid Atlantic & Appalachia
Examining how seven Mid-Atlantic and Appalachian jurisdictions balance federal Medicaid work mandates with deep-rooted economic disparities, rural health gaps, and political crosscurrents.
14D: Mountain West
A comprehensive analysis of how eight Mountain West states confront federal Medicaid work mandates while grappling with tribal sovereignty, vast frontier landscapes, tourism-driven economies, and persistent rural health disparities.
14E: Northeast
Eight Northeastern states face a new reality: implementing federal Medicaid work requirements while contending with aging populations, dense urban cores, rural isolation, immigrant diversity, and political resistance.
14F: Pacific West
Five Pacific states confront the federal Medicaid work requirement mandate, balancing vast geographic challenges, cultural diversity, and progressive policy traditions against the risk of widespread coverage disruption.
14G: Plains
Medicaid work requirements in the Plains states reveal a spectrum of approaches shaped by labor shortages, rural healthcare fragility, political dynamics, and unique demographic challenges.
14H: Southeast
Medicaid work requirements in the Southeast reflect a clash of ideology, tight timelines, and fragile infrastructure, producing uneven coverage outcomes amid rural hospital crises, seasonal employment, and persistent racial health disparities.
15A: Allostatic Load and Administrative Burden
Administrative burden does more than create obstacles, it triggers chronic stress responses that harm health and turn systems intended to heal into sources of damage.
15B: The Executive Function Paradox
As many Medicaid beneficiaries struggle with poverty-related cognitive load and conditions like ADHD and depression, work requirements impose planning, memory and organizational demands that exceed their capacity, creating a system that fails not from unwillingness but from structural mismatch.
15C: Behavioral Design for Compliance Systems
When defaults, timing, and friction reduction guide policy, coverage loss becomes preventable.
15E: The Caseworker's Dilemma
How rigid rules collide with ethics, leaving caseworkers torn between duty and values.
15F: Macro Practice and System Change
Why linking individual navigation to systemic advocacy is essential for social work’s commitment to justice.
15G: Bureaucracy and the Reproduction of Inequality
Bureaucratic work requirement systems promise neutrality but embed rules, burdens, and institutional logics that sort populations by administrative capacity, reproducing inequality through structural design.
15H: Networks, Capital, and Compliance
When networks, capital, and compliance collide, hidden resources determine who keeps coverage and who loses it
15I: How People Actually Navigate Systems
Inside the real world of compliance: the waiting rooms, improvised strategies, and cultural logics that policy overlooks.
15J: Dignity, Autonomy, and the Ethics of Conditionality
Conditioning healthcare on behavior is not just policy, it is a moral stance on dignity, reciprocity, and the limits of state power.
15K: The Long Arc of Work-Conditioned Benefits
When centuries of moral judgment echo through policy, work requirements reveal the long arc of conditional care.
15L: The Spatial Politics of Compliance
Uniform work requirements meet unequal infrastructure, turning geography into a hidden determinant of coverage.
16A: The Political Economy of State Variation
A deep dive into why states implement Medicaid work requirements differently and how politics, fiscal realities, and administrative capacity shape the spectrum from permissive to punitive.
16B: The Advocacy Ecosystem
The organizations fighting for and against Medicaid work requirements, and the stakeholders caught in between.
16C: The 2026 Midterm Context
How the 2026 midterm elections collide with Medicaid work requirement implementation and why timing, oversight, and campaign strategy shape political stakes.
16D: Media Framing and Public Opinion
Media framing and public opinion shape whether Medicaid work requirements are viewed as common-sense accountability or harmful barriers to healthcare access.
16E: Litigation as Policy Tool
When court battles redefine Medicaid work requirements, legal challenges shift from blocking policy to shaping implementation under OB3.
16F: Federal-State Dynamics
How presidential administrations and CMS discretion shape what states can do.
16G: Policy Feedback and Political Sustainability
When Medicaid work requirements move from debate to implementation, policy feedback mechanisms will determine whether they spark backlash, normalize, or remain contested.
16H: Interest Group Dynamics
Interest group dynamics reveal how MCOs, hospitals, providers, employers, and state agencies quietly shape Medicaid work requirement implementation through alliances and conflicting incentives.
17A: Risk Adjustment Models in Medicaid Managed Care
When Medicaid work requirements take effect in December 2026, states’ risk adjustment methodologies will play a pivotal role in shaping managed care payments and financial strategies for MCOs and ACOs.
17B: Fee-for-Service Versus Managed Care in Medicaid Expansion
Exploring how Medicaid expansion delivery systems determine states’ readiness for work requirements and the administrative burden ahead.
17C: Medicaid ACO Models and Work Requirements
How Medicaid ACOs must adapt payment models and retention strategies as OB3 work requirements destabilize attribution, benchmarks, and long-term investment returns.
17D: The Fiscal Foundation: Federal Matching, State Shares, and the Architecture of Medicaid Finance Under OB3
When OB3 reshapes Medicaid financing, states face mounting costs, provider tax restrictions, and unfunded mandates that threaten coverage stability and implementation capacity.

